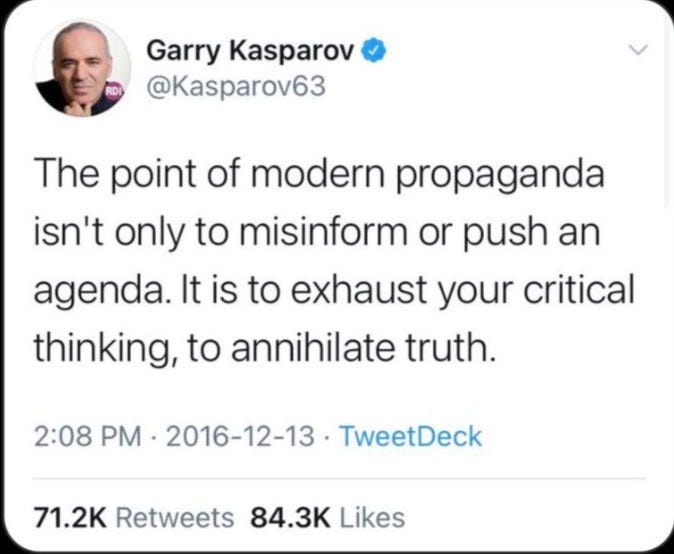
Plus ça change plus c'est la même chose
Benefits quite difficult to see, mechanism of action unknown, but do it anyway. Clot shot anyone?
While a certain false equivalence may exist here, a point nevertheless stands.
I recall an item on the New Zealand National Radio News extolling the expansion of prescribing rights for SSRIs from the specialist domain to general practice in 1997. This was back in the day when I listened with half an ear, before Radio NZ “The Our News” became the fully integrated, well greased State propaganda unit of today demanding to be irrevocably silenced.
I remember listening to an interveiwed spokesman for the RNZCGP reassuring listeners that the use of this new class of anti-depressants (SSRIs) in general practice would be very carefully prescribed and monitored.
The skeptic in me squirmed; ‘Smarties’ just wouldn’t come into it. At the time I remember reflecting that it sounded like the starting bell of an incipient re-run of the global prescription of antibiotics ~ and we all know how that race ended.
And so, as time went by, the data and comments accumulated. The following is a jaundiced ad hoc selection from across the years. Bias is on full noise.
There were substantial variations between drugs in the level of association with fatal poisoning. Assuming an average treatment episode lasted three months, one SSRI fatality is associated as a group with one in 411,800 (95% CI = 243,300 to 1.34 million) (Mason J, Freemantle N, Eccles M, 2000)
The most prominent type of depression that GPs believed they were treating was ‘chronic mild depression’, which contrasts with the subsidized indication for all newer antidepressant classes of ‘major depressive disorders’. (McManus P, Mant A, Mitchell P et al. 2003)
For adolescents or children with depression the UK report confirms the earlier recommendations against all SSRIs being used apart from fluoxetine (Prozac) where there is some evidence of overall benefit. However the report warns that this drug too, like other SSRIs, is likely to be linked with a small increased risk of self harm or suicidal thoughts. The UK report reiterates that while there is no clear evidence of an increased risk of self harm and suicidal thoughts in young adults aged 18 and over, careful monitoring is recommended. It says patients in this age group are at increased risk of suicidal thinking and action than other age groups with depression. (Medsafe 7 Dec 2004 UK Antidepressant Report Reinforces NZ Actions)
Age, gender and pre-existing depression/suicidal ideation are important confounders in observational studies of the association between antidepressants and suicide or self harm. (Didham RC, Doug W. McConnell DW, Blair HJ et al. 2005)
The research clearly shows that the prescribing of antidepressants in New Zealand has significantly increased since 1997, the proportion of the population prescribed an antidepressant varies significantly between DHB regions, the intensity of prescribing is at levels at the low end of the adult treatment range recommended by Medsafe, and there is an observed small increased risk of hospitalisation for intentional self-harm and the prescribing of nortriptyline, paroxetine and fluoxetine after adjusting for a range of population-level confounders. (Ministry of Health. 2007. Patterns of Antidepressant Drug Prescribing and Intentional Self-harm Outcomes in New Zealand: An ecological study. Wellington: Ministry of Health.)
Recent studies suggest that SSRI antidepressant use in pregnancy may increase the risk of congenital abnormalities. There is also evidence to suggest that use of these medicines in later stages of pregnancy can lead to neonatal complications indicative of a withdrawal syndrome, and to persistent pulmonary hypertension of the newborn. Whether this observed increase in risk is attributable to SSRIs or to other confounding factors requires further analysis. Nonetheless, this new research suggests there may be an association between SSRIs and congenital malformations; this appears to be strongest for paroxetine and club foot, neural tube defects and cardiovascular abnormalities. In a recent case-control study, maternal use of SSRIs after the first 20 weeks of pregnancy was associated with an increase in the risk of persistent pulmonary hypertension of the newborn (PPHN). Further investigation of this association is warranted; however, on the basis of this study, the absolute risk of PPHN among those who use SSRIs late in pregnancy is approximately 6 to 12 per 1000 women. This compares to 1 to 2 cases of PPHN per 1000 women in the general population. (2008 Medsafe Update 29(1): 7-8)
The 12 month prevalence of antidepressant dispensing among the total population aged 15-100 years increased from 7.36%% in 2004-2005 to 8.21%% in 2005-2006 and to 9.39%% in 2006-2007 Selective serotonin re-uptake inhibitor (SSRI) and tricyclic antidepres-sants (TCA) accounted for >90% of all antidepressants dispensed each year. SSRIs were more frequently prescribed to young adults (15-24 years) than TCAs, although this relation changed with increasing age. (Exeter D, Robinson E, and Wheeler W, 2009)
Antidepressant prescribing continues to increase, with 5-16% of adults receiving antidepressants annually. Total prescribing growth is due in part to increased long-term use, greater selective serotonin re-uptake inhibitor (SSRI) use and the use of higher SSRI doses. Evidence does not support routine use of higher SSRI doses for depression treatment, and factors influencing the use of such doses are not well known. (Johnson, C.F., Williams, B., MacGillivray, S.A. et al. 2017)
However, Prof Healy told a global health conference in Aberdeen that - in 29 paediatric clinical trials of antidepressants - every single one failed to produce an obvious benefit. He said: "At the same time, in every single one of these trials it has produced more harms than benefits in the sense that it has made children become suicidal who wouldn't have become suicidal if they hadn't been put on these drugs. We have a situation where if you are following the evidence no-one should be using these drugs. At the same time, in teenagers, these drugs have become the most commonly used drugs." Figures obtained by the BBC showed the number of children under 18 being prescribed antidepressants doubled from 2,748 in 2009/10 to 5,572 in 2016. The number of children under 13 given antidepressants went up from 57 to 252 in the same period. The statistics showed 45% of the under-18s were prescribed fluoxetine, which is usually sold under the trade name Prozac. (5 February 2018 Teenage antidepressants 'doing more harm than good' By Shelley Jofre BBC Scotland health correspondent)
In New Zealand, its estimated one in nine adults are prescribed antidepressants each year with the number of prescriptions thought to be rising at five percent per annum. The results point to a significant number of people prescribed antidepressants who have experienced some withdrawal effects and who believe the drugs are addictive. (June 2018, NZ Doctor citing U.AKL study)
In New Zealand the number of annual recipients for people aged 15 or over increased by 21% from 2008 to 2015, in which year 13% of all New Zealanders were prescribed an antidepressant (16% of females and 9% of males) (Read, J., Gibson, K., Cartwright (2021) citing, C.Wilkinson & Muller, (2018))
The three ADs [anti-depressants] most commonly prescribed by GPs were: citalopram (32.6%), fluoxetine (28.4%) and paroxetine (13.3%). The three ADs most commonly prescribed by Psychiatrists were: fluoxetine (23.7%), citalopram (22.6%) and venlafaxine (20.8%) (Read, J., Gibson, K., Cartwright C., 2021)
A meta-analysis found that ‘the overall effect of new-generation antidepressant medications is below recommended criteria for clinical significance’ (Kirsch et al. 2008, p. 265) with no benefit compared to placebo for all but a tiny minority of recipients, namely ‘patients at the upper end of the very severely depressed category’ (p. 260). There is evidence that antidepressants are no more effective than placebo in anyone - regardless of severity. Moncrieff and Kirsch (2015) have shown that the differences (even those in people with severe depression) are well below empirically evidenced criteria for clinical relevance. (Read, J., Gibson, K., Cartwright C., 2021; pp2)
And So Here We All Are
This latest from the Goodfellow Unit who assert their GEMS are “…either practice changing or thought provoking.” (2022, Sep 14).
Indeed.
Nota bene
“This does not mean that SSRIs do not work, more that we don’t have a good understanding of their mechanism of action.”
PostScript
This does not mean that Pfizer mRNA / lipid nano-particle shots do not work, more we don’t have a good understanding of their mechanism of action.